Pharmacological interventions
What you should know about drugs and why
Some basic knowledge about pharmacological interventions is important for you as a professional involved in the management of dementia, even if you are not a physician. You need to understand how the drugs work, what their potentials, risks and side effects are, and how they can be used to improve the quality of life of people with dementia. It is equally important to appreciate that pharmaceuticals are only a basis of the management of dementia, that their effects are limited and that pharmacological treatments need to be complemented by non-pharmacological interventions.
Types of pharmaceutical agents used in dementia
Only two types of pharmacologicals have been specifically approved for the improvement or stabilisation of cognitive symptoms and activities of daily living in dementia: cholinesterase inhibitors and memantine (“antidementia drugs”). Other classes of drugs are used to treat behavioural symptoms such as apathy, agitation, delusions or hallucinations. These pharmaceuticals include antidepressants and antipsychotics and are also used in other conditions than dementia.
Pharmacological agents used in the treatment of dementia
| Category | Chemical type (examples) | Target symptoms |
| Antidementia drugs | Cholinesterase inhibitors Memantine | Memory, attention Activities of daily living |
| Antidepressants Antipsychotics | Selective serotonin reuptake inhibitors (SSRI) Atypical antipsychotics | Behavioural problems |
Anti-dementia drugs
Cholinesterase inhibitors and memantine are used to treat key symptoms of dementia such as impairment of memory and attention or decline of activities of daily living. They work on chemical compounds which are used in the brain for the communication between nerve cells (neurotransmitters). Cholinesterase inhibitors partially restore the deficit in acetylcholine, particularly in Alzheimer’s and Lewy body diseases. Three cholinesterase inhibitors are approved for the treatment mild and moderate (not severe) dementia in Alzheimer’s disease: donepezil, galantamine, rivastigmine. These drugs are interchangeable in case of side effects or questionable treatment response. Rivastigmine is available as a once-daily skin patch which offers better tolerability than the capsule formulation. Memantine attenuates the toxic effects of glutamate which is released in excessive amounts from degenerating nerve cells. Memantine is approved for moderate to severe dementia in Alzheimer‘s disease. Neither antidementia drug is approved for the treatment of mild cognitive impairment.

How do anti-dementia drugs work?
There are two signalling chemicals (neurotransmitters) that contribute to the proper functioning of the brain: acetylcoline and glutamate. In Alzheimer’s disease and Lewy body disease acetylcholine-producing cells which are located deep the brain go away early, resulting in a significant shortage of acetylcholine. Glutamate is synthesised by nerve cells in the outermost parts of the brain. When these cells degenerate excessive and noxious amounts of glutamate are released on neighbouring cells. The amount of acetylcholine in the brain can be increased by blocking the enzyme that inactivates it (cholinesterase). Memantine attenuates the toxic effects of excess glutamate by blocking the receiving sites (receptors).


What are the effects and side effects of anti-dementia drugs?

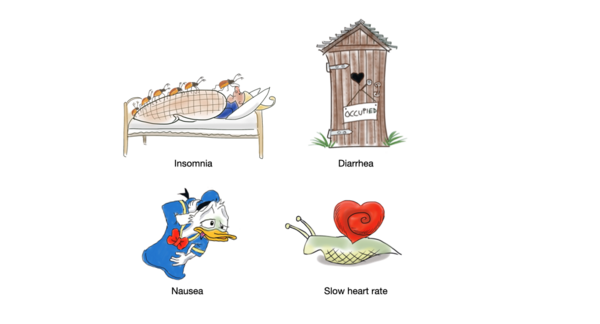
Cholinesterase inhibitors do not improve cognitive abilities or activities of daily living to a large extent, but rather slow down the progression of these symptoms for about one year. The most frequent side effects are nausea, vomiting, diarrhoea, insomnia and slowing of the heart rate. Memantine has similar but somewhat weaker effects. Side effects of Memantine such as dizziness and headache are rare. Since the two types of drugs work by different mechanisms they can be combined to increase efficacy.
How can the efficacy of anti-dementia drugs be determined?
To evaluate the efficacy of cholinesterase inhibitors or memantine, cognitive functions and activities of daily living should be repeatedly assessed using cognitive tests (e.g. the Mini Mental State Examination – MMSE) and interviews with carers. The reimbursement of antidementia drugs by health insurances usually depends on the results of such a monitoring. Either improvement or stabilisation must be demonstrated.
Antidepressants and antipsychotics
During the course of illness, more than 80 percent of people with dementia develop behavioural symptoms which may require treatment. If possible, non-pharmacological interventions should be used first. However, if the behavioural symptoms are severe or dangerous for the person or others, drug treatment cannot be avoided. For the treatment of depression or apathy antidepressants may be tried. Modern drugs (e.g. citalopram, sertraline, trazodone, mirtazapine) should be preferred to older pharmaceuticals Other types of behavioural change such as agitation, delusions or hallucinations may require treatment with antipsychotics. The problem with antidepressants and antipsychotics is that they have severe side effects including cerebrovascular accidents (stroke) and increased mortality (risk of death). Newer (atypical) antipsychotics (e.g. risperidone, quetiapine) should be used instead of older compounds. People with dementia in Lewy body disease are particularly vulnerable to the side effects of antipsychotics.
References
- Cummings J, Gee G, Ritter A et al. Alzheimer’s disease drug development pipeline: 2020. Alzheimer’s Dement 6: e12050, 2020
- Hampel H, Mesulam MM, Cuello AC,et al. The cholinergic system in the pathophysiology and treatment of Alzheimer's disease. Brain 141: 1917–1933, 2018
- Hort J, O'Brien JT, Gainotti G, Pirttila T, Popescu BO, Rektorova I, Sorbi S, Scheltens P. EFNS Scientist Panel on Dementia: EFNS guidelines for the diagnosis and management of Alzheimer's disease. Eur J Neurol 17,1236-48, 2010
- Knopman DS, Jones dT, Greicius MD. Failure to demonstrate efficacy of aducanumab: An analysis of the EMERGE and ENGAGE trials as reported by Biogen, December 2019. Alzheimers Dement 17: 696-701, 2021
- Raina P, Santaguida P, Ismaila A, Patterson C, Cowan D, Levine M, Booker L, Oremus M. Effectiveness of cholinesterase inhibitors and memantine for treating dementia: evidence review for a clinical practice guideline. Ann Intern Med 148: 379–397, 2008
- Reisberg B, Doody R, Stöffler A, et al. Memantine Study Group: Memantine in moderate-to-severe Alzheimer’s disease. N Engl J Med 348: 1333–1341, 2003
- van de Glind EMM, van Enst WA, van Munster BC et al. Pharmacological treatment of dementia: a scoping review of systematic reviews. Dement Geriatr Cogn Disord 36: 211–228, 2013
- Winblad B, Engedal K, Soininen H, et al. A 1-year, randomized, placebo-controlled study of donepezil in patients with mild to moderate AD. Neurology 57: 489-495, 2001
- Yiannopoulou KG, Papageorgiou, SG. Current and Future Treatments in Alzheimer Disease: An Update. J Cent Nerv Syst Dis 12, 1179573520907397, 2020
