Disclosure of diagnosis
Why is disclosure of the diagnosis so important?
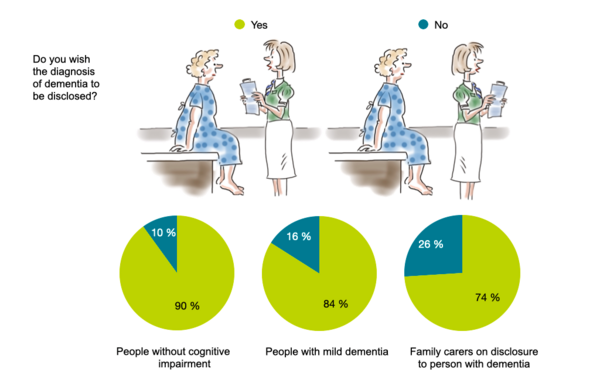
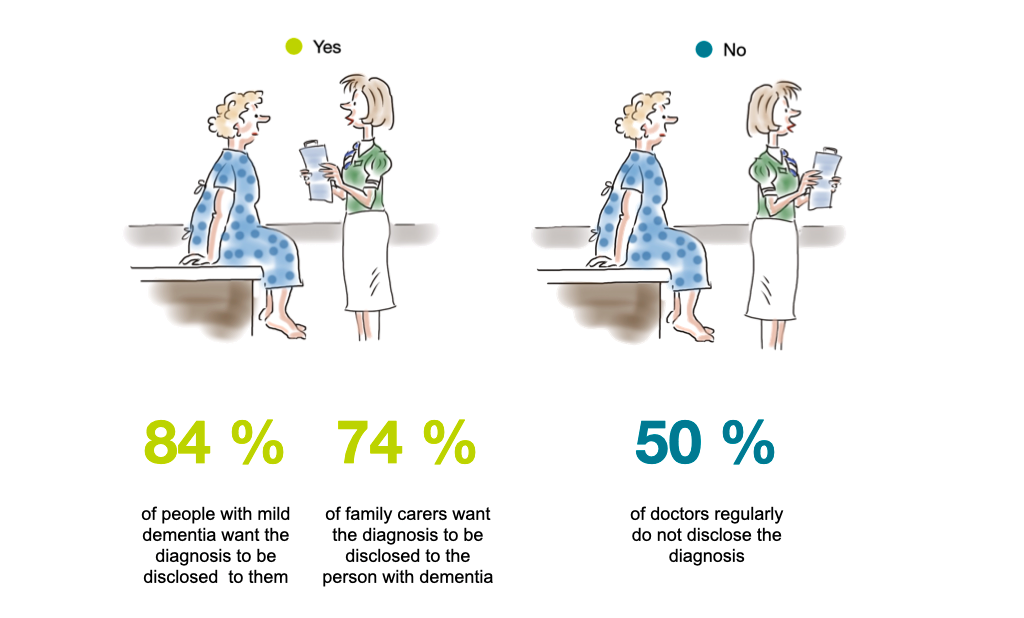
Most people with dementia and the majority of carers wish to be informed about the diagnosis. Over 90 % of individuals without cognitive impairment are in favour of disclosure if they were to develop dementia; among those already diagnosed with dementia, the rate was 84 %. Interestingly, only 74 % of informal carers want the diagnosis to be disclosed to the person with dementia.
The major reasons for the positive attitudes regarding disclosure are the opportunity to plan, receive treatment, obtain information, and learn coping strategies. The main arguments against disclosure are that it would upset or depress, and that there are no benefits in knowing.
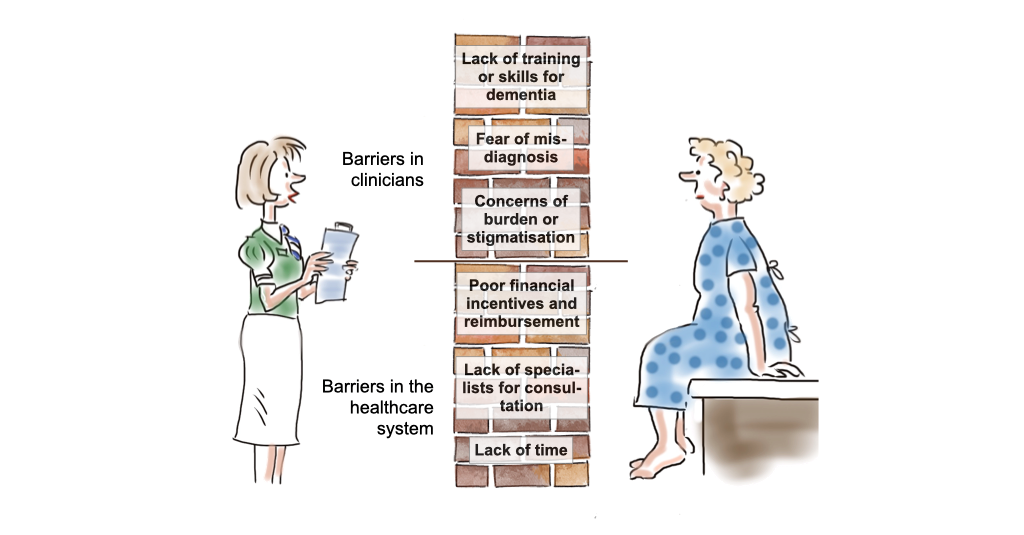
However, there is a marked discrepancy between the preferences of people with dementia and the practice of physicians. Around 50 % of clinicians routinely withhold a dementia diagnosis. Physicians’ barriers to diagnosis include low confidence in their ability to diagnose dementia, fear to violate the physician-patient relationship, concerns that the person with dementia would not understand the diagnosis, fear to harm the person with dementia, and the belief that no effective treatment is available.
It is not only timely diagnosis, but also timely disclosure that helps a person take decisions and maintain their quality of life.
Factors affecting disclosure
Even if it has been disclosed, the diagnosis is often not recalled by people with dementia. This is not only due to cognitive impairment, but also to insufficient clarity of communication, too technical language, information flooding, or emotional overload. When telling the diagnosis, it is essential to consider how well the person can process the information, what they already know about their condition, what they wish to know and what not.
People with dementia may not be aware of their diagnosis even if it has been disclosed to them.
Examples: Experiences of people with dementia with disclosure
Emily: I received the diagnosis at the second visit. It was important for me that a doctor asked if I wish to be there alone or with my family.
Daniel: I was able to ask a few questions – which was helpful. I struggled a little with the language the doctor used. I wished he used a language that was easier to understand.
Peter: I could not believe it when a doctor told me the diagnosis. I needed time to absorb it. I was glad that she respected that I was shocked. She offered me to see her in a few days and to talk things over when I would be ready.
Examples: Experiences of professionals with disclosure
At the beginning of my career as a general practitioner I was very unsure how to disclose the diagnosis of dementia. Especially, because I couldn’t offer a cure and I didn’t want to cause even more despair in people with dementia. But over time I found ways how to improve my skills regarding disclosure.
I always take at least 20 minutes for the disclosure and I address it also in the second visit.
Prior to the conversation, I think about the background, knowledge and expectations of the patient.
I start the conversation by saying: „Here are the results of your examination that may explain the problems that you are experiencing“.
I address the emotions that come up after telling the diagnosis. I say „I understand that this is difficult news for you.“
I am ready to answer the questions of a patient and their family.
I provide additional contacts and recommendations for professionals who may be of help.
How to disclose the diagnosis of dementia?
The style of disclosing the diagnosis must be individualized and take into consideration the previous knowledge (including misperceptions), informational needs and emotional state of the person. It requires a great deal of skillful communication. If possible, the disclosure of diagnosis should not be a single event where all information is shared at once, but be arranged as a staged process.
Preparation
- Ask the person whether they wish to be told the diagnosis and whether their loved ones should also be informed
- Explore knowledge, beliefs and perceptions about the diagnosis
- Probe assumptions of the person by asking questions such as „What do you think causes the change in your memory?“ or „What do you suspect the results of testing might show?“
Meeting information needs
- Use a non-technical language that the person with dementia understand
- Provide comprehensive information including areas of uncertainty, treatment options, resources of help and what lies ahead
- Allow time for questions and discussion
- Follow up after disclosure to make sure that the information has been taken up
- Provide additional written material to the person and the family
Meeting emotional needs
- Reflect back to the person by saying: „I imagine this is difficult news“ or similar
- Maintain hope by telling the person that many abilities will be preserved and need to be uncovered and used
- Encourage coping with the diagnosis and promote future planning
- Confirm your commitment to ongoing care
- Use the word „dementia“ with caution; explain the medical use of the term.
References
- Carpenter B, Dave J. Disclosing a dementia diagnosis: A review of opinion and practice, and a proposed research agenda. Gerontologist 44: 149-158, 200
- Cornett PF, Hall JR. Issues in disclosing a diagnosis of dementia. Arch Clin Neuropsychol 23: 251-256, 2008
- Frank C, Forbes RF. A patient’s experience in dementia care. Can Fam Physician 63: 22-26, 2017
- Mastwyk M, Dow B, Ellis KA, Ames D. Why attend a memory clinic? What do patients and their families want and/or expect? Australas J Ageing 35: 220-224, 2016
- Pinner G, Bouman W. Attitudes of patients with mild dementia and their carers towards disclosure of the diagnosis. Int Psychogeriatr 15: 279-288, 2003
- Smith AP, Beattie BL. Disclosing a diagnosis of Alzheimer’s disease: patient and family experiences. Can J Neurol Sci 28 (Suppl 1): S67-71
- van den Dungen P, van Kuijk L, van Marwijk H, et al. Preferences regarding disclosure of a diagnosis of dementia: a systematic review. Int Psychogeriatr 26: 1603-1618, 2014.
- Whitehouse P, Frisoni GB, Post S. Breaking the diagnosis of dementia. Lancet Neurol 3: 124-128, 2004.
- Wilkinson H, Milne AJ. Sharing a diagnosis of dementia--learning from the patient perspective. Aging Ment Health 7: 300-307, 2003
